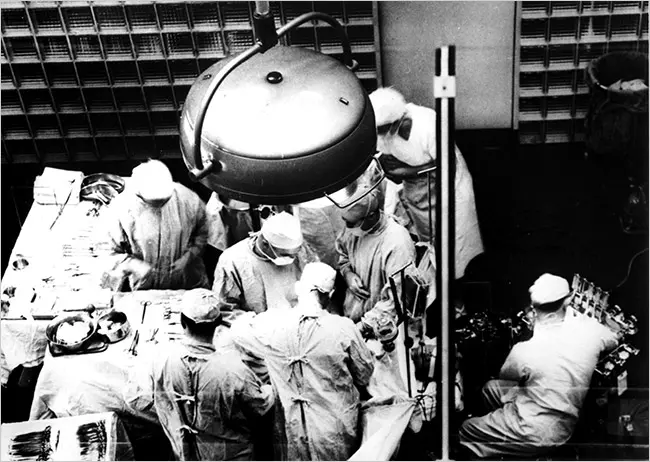
Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.
Organs that have been successfully transplanted include the heart, kidneys, liver, lungs, pancreas, intestine, thymus and uterus. Tissues include bones, tendons (both referred to as musculoskeletal grafts), corneae, skin, heart valves, nerves and veins. Worldwide, the kidneys are the most commonly transplanted organs, followed by the liver and then the heart. Corneae and musculoskeletal grafts are the most commonly transplanted tissues; these outnumber organ transplants by more than tenfold.
Organ donors may be living, brain dead, or dead via circulatory death. Tissue may be recovered from donors who die of circulatory death, as well as of brain death – up to 24 hours past the cessation of heartbeat. Unlike organs, most tissues (with the exception of corneas) can be preserved and stored for up to five years, meaning they can be "banked". Transplantation raises a number of bioethical issues, including the definition of death, when and how consent should be given for an organ to be transplanted, and payment for organs for transplantation. Other ethical issues include transplantation tourism (medical tourism) and more broadly the socio-economic context in which organ procurement or transplantation may occur. A particular problem is organ trafficking.[5] There is also the ethical issue of not holding out false hope to patients.
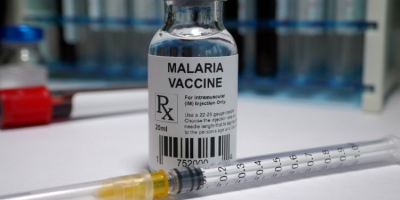
Transplantation medicine is one of the most challenging and complex areas of modern medicine. Some of the key areas for medical management are the problems of transplant rejection, during which the body has an immune response to the transplanted organ, possibly leading to transplant failure and the need to immediately remove the organ from the recipient. When possible, transplant rejection can be reduced through serotyping to determine the most appropriate donor-recipient match and through the use of immunosuppressant drugs.
Credit : Wikipedia
Picture Credit : Google