How does the stomach work?
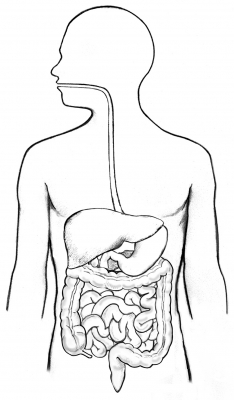
The stomach is a muscular hollow organ. It takes in food from the esophagus (gullet or food pipe), mixes it, breaks it down, and then passes it on to the small intestine in small portions.
The entire digestive system is made up of one muscular tube extending from the mouth to the anus. The stomach is an enlarged pouch-like section of this digestive tube. It is located on the left side of the upper abdomen and shaped somewhat like an oversized comma, with its bulge pointing out to the left. The stomach’s shape and size vary from person to person, depending on things like people’s sex and build, but also on how much they eat.
At the point where the esophagus leads into the stomach, the digestive tube is usually kept shut by muscles of the esophagus and diaphragm. When you swallow, these muscles relax and the lower end of the esophagus opens, allowing food to enter the stomach. If this mechanism does not work properly, acidic gastric juice might get into the esophagus, leading to heartburn or an inflammation.
The upper-left part of the stomach near the opening curves upward towards the diaphragm. This part is called fundus. It is usually filled with air that enters the stomach when you swallow. In the largest part of the stomach, called the body, food is churned and broken into smaller pieces, mixed with acidic gastric juice and enzymes, and pre-digested. At the exit of the stomach, the body of the stomach narrows to form the pyloric canal, where the partially digested food is passed on to the small intestine in portions.
The stomach wall is made up of several layers of mucous membrane, connective tissue with blood vessels and nerves, and muscle fibers. The muscle layer alone has three different sub-layers. The muscles move the contents of the stomach around so vigorously that solid parts of the food are crushed and ground, and mixed into a smooth food pulp.
The inner mucous membrane (lining) has large folds that are visible to the naked eye. These folds run toward the exit of the stomach, providing “pathways” along which liquids can quickly flow through the stomach. If you look at the mucous membrane under a microscope, you can see lots of tiny glands. There are three different types of glands. These glands make digestive enzymes, hydrochloric acid, mucus and bicarbonate.
Gastric juice is made up of digestive enzymes, hydrochloric acid and other substances that are important for absorbing nutrients – about 3 to 4 liters of gastric juice are produced per day. The hydrochloric acid in the gastric juice breaks down the food and the digestive enzymes split up the proteins. The acidic gastric juice also kills bacteria. The mucus covers the stomach wall with a protective coating. Together with the bicarbonate, this ensures that the stomach wall itself is not damaged by the hydrochloric acid.
Credit : NCBI
Picture Credit : Google