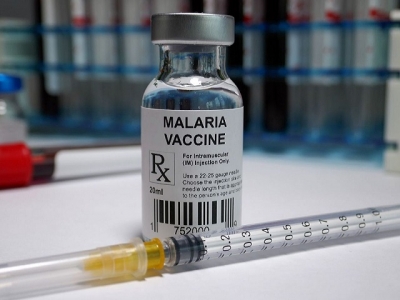
October 6, 2021, marks a historic day in humanity's fight against malaria, as the World Health Organization (WHO) approved the rollout of the malaria vaccine, RTS.S/AS01 (RTS.S) among children living in sub-Saharan Africa and other at-risk regions.
Malaria is a deadly infectious disease that claims more than 4 lakh lives every year around the world. It is caused by Plasmodium parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes, called the malaria vector. Among the five parasite species that cause malaria in humans, Plasmodium falciparum and Plasmodium vivax pose the greatest threat.
Who will get the vaccines and how efficient is it in preventing the spread of malaria?
WHAT is RTS,S/AS01?
RTS,S/AS01 or Mosquirix (trade name) has been developed by British drug manufacturer GlaxoSmithKline in collaboration with Seattle-based health non-profit PATH and a network of African research centres, with partial funding from the Bill and Melinda Gates Foundation. The vaccine is the result of 30 years of research and it targets Plasmodium falciparum, the most common parasite causing malaria in Africa. The vaccine offers no protection against the other four species such as P vivax, P ovale, P knowlesi and P malariae which are prevalent in Southeast Asia, Americas and Europe.
RTS,S was created in 1987 by scientists working in GlaxoSmithKline laboratories. The European Medicines Agency issued a positive scientific opinion on the vaccine in July 2015, concluding that the benefits of the vaccine outweigh the risks
RTS.S has been rigorously tested through a series of clinical trials since 2019 in seven African countries (Burkina Faso, Gabon, Ghana, Kenya, Malawi, Mozambique, and Tanzania).
Who is it for?
The WHO has recommended that the RTS,S/AS01 malaria vaccine be used for the prevention of P. falciparum malaria in children living in regions with moderate to high transmission as defined by it. The vaccine has been recommended to be provided in a schedule of four doses in children from 5 months of age.
What is its efficacy?
The current approval of the vaccine is based on the results of the ongoing pilot programme in Ghana, Kenya and Malawi. More than 2.3 million doses of the vaccine have been administered in these countries so far as part of the pilot. The following observations have been made since:
- The vaccine offers 39% protection against malaria in children between the ages of five and 17 months.
- The vaccine prevents approximately 4 in 10 (39%) cases of malaria and about 3 in 10 (29%) cases of severe malaria.
- There is significant reductions in overall malaria admissions as well as malaria-induced anaemia.
- The vaccine also reduced the need for blood transfusions, which are required to treat life-threatening malaria anaemia by 29%.
How does the vaccine work?
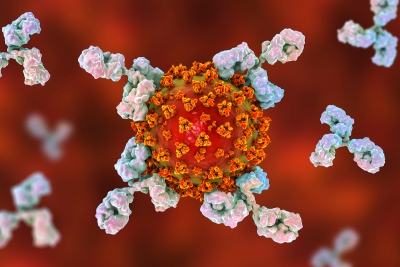
RTS,S works by introducing the immune system to a fragment of a protein that is naturally present on the surface of Plasmodium parasite when it enters the bloodstream through an infected mosquito. The protein in the vaccine stimulates the production of antibodies, and allows the body to mount a swift response to the parasite the next time it is encountered. The vaccine is designed to prevent the parasite from infecting the liver, where it can mature, multiply, re-enter the bloodstream, and infect red blood cells, which can lead to disease symptoms.
Why is developing a vaccine against malaria tough?
Malaria vaccines have been in development since the 1960s, with substantial progress only in the last decade.
- Developing a vaccine against malaria parasite has been a difficult task, chiefly because of the parasite's complex lifecycle and genetical make-up. It has a multistage lifecycle occurring within two living beings, the vector mosquitoes and the vertebrate hosts (humans for instance). The survival and development of the parasite within the invertebrate and vertebrate hosts, in intracellular and extracellular environments, is made possible by more than 5,000 genes and their specialised proteins that help the parasite to invade and grow within multiple cell types and to evade host immune responses. The surface proteins and metabolic pathways keep changing during these different stages, that help the parasite to evade the immune clearance, while also creating problems for the development of drugs and vaccines.
- The technical complexity of developing any vaccine against a parasite is another obstacle.
- With no real market for a malaria vaccine in resource-rich countries like the U.S., pharmaceutical companies did not have a strong financial incentive to accelerate vaccine development. Hence there are a few malaria vaccine developers.
What are the symptoms and consequences of malaria?
Symptoms usually appear 10-15 days after the infective mosquito bite. According to the WHO, the first symptoms-fever, headache, and chills - may be mild and difficult to recognise as malaria. In no time, it can progress into severe illness and possible death.
Children may develop severe anaemia, respiratory distress or cerebral malaria, while adults can face multi-organ failure. Children under 5 years of age are the most vulnerable group affected by malaria.
Some facts about malaria
- There are more than 400 species of Anopheles mosquito, of which around 30 are malaria vectors. All the important vector species bite between dusk and dawn.
- Anopheles mosquitoes lay their eggs in water, usually shallow pools of fresh water, such as puddles, which are abundant during the rainy season in tropical countries. .
- Vector control is the main way to prevent and reduce malaria transmission. The two WHO-recommended methods are - insecticide-treated mosquito nets and indoor residual spraying. Early diagnosis and treatment of malaria reduces disease and prevents deaths.
- Exposure to malaria parasites does not confer lifelong protection.
Picture Credit : Google